For behavioral health providers running Intensive Outpatient (IOP) and Partial Hospitalization Programs (PHP), the word “audit” can trigger immediate anxiety. Even high-performing programs—those delivering excellent care and strong outcomes—often worry whether their documentation will stand up to payer scrutiny, state reviews, or accreditation audits.
That stress usually isn’t about clinical quality. It’s about documentation risk.
IOP and PHP programs generate enormous volumes of information: daily attendance, group therapy notes, treatment plans, authorizations, utilization reviews, level-of-care decisions, and discharge summaries. When that data lives across spreadsheets, shared drives, and disconnected EHR modules, audits turn into a frantic scavenger hunt.
The reality is this: audit-ready documentation isn’t created during an audit—it’s built into daily workflows.
With the right systems and structure, audits stop being a threat and start becoming a confirmation that your program is doing exactly what it should. This is how documentation that stands up is created—and how Valant helps programs get there.
What Audit-Ready Documentation for IOP and PHP Really Looks Like
Audit-ready documentation tells a clear, consistent story of care from admission through discharge. It shows that services were medically necessary, authorized, delivered as planned, and appropriately adjusted over time.
For IOP and PHP programs, that means documentation that consistently connects:
- Admission criteria and level-of-care placement
- Treatment plans tied to diagnoses and goals
- Daily attendance and participation
- Utilization review and authorization management
- Clinical progress and adjustments
- Discharge planning and step-down care
A behavioral health EHR that supports audit readiness doesn’t ask clinicians or staff to “remember” compliance. Instead, it guides teams to capture required elements as care is delivered, with documentation and workflows linked within the EHR. That’s the difference between documentation that exists and documentation that meets compliance standards when it matters.
Common Payer Requirements for IOP Documentation (and How to Build Them In)
While payer requirements vary, most IOP and PHP audits focus on a familiar set of expectations:
- Clear medical necessity for the level of care
- Treatment plans aligned to diagnoses and goals
- Evidence of patient participation and progress
- Attendance that matches billed services
- Authorizations that align with services delivered
- Timely and complete discharge documentation
Problems arise when these elements are documented inconsistently—or worse, in different systems.
Valant’s approach is to support documentation templates and workflows that align with common payer expectations for IOP and PHP programs. Instead of free-text notes that vary by clinician or location, structured templates help teams capture required elements consistently—without sacrificing clinical nuance. This reduces audit risk while also making documentation faster and more intuitive for staff.
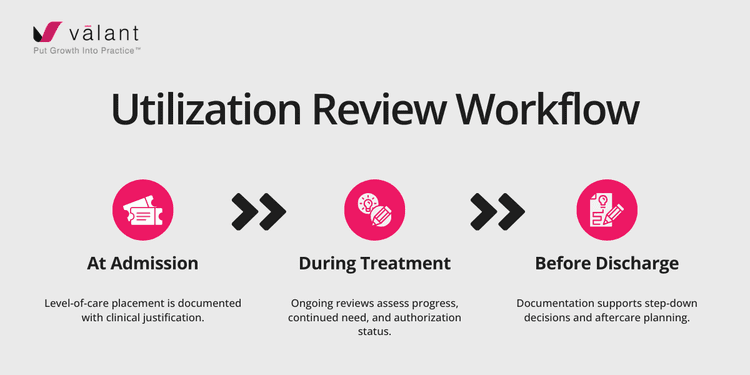
What an Effective Utilization Review Workflow Looks Like
Utilization review is one of the most scrutinized areas in IOP and PHP audits. Payers want to see that services were:
- Authorized
- Medically necessary
- Provided at the appropriate intensity
- Adjusted when patient needs changed
An effective utilization review workflow spans the entire episode of care:
When utilization review lives outside the EHR—in emails, spreadsheets, or payer portals—gaps are inevitable. When it’s built into the EHR, authorization status, clinical justification, and service delivery remain aligned at every step.
This alignment is critical not just for audits, but for sustainable program growth.
Preventing Overutilization Without Compromising Care
Overutilization is one of the fastest ways to trigger payer scrutiny. But underutilization carries its own risks—both clinically and financially.
The goal isn’t to limit care. It’s to deliver the right level of care, for the right duration, with clear justification.
With the right EHR tools, teams can use timely, connected data to:
- Track authorized units alongside attendance
- Monitor utilization trends across patients and programs
- Identify when services are nearing authorization limits
- Adjust treatment intensity based on documented progress
This allows providers to meet patient needs while staying compliant—without relying on manual tracking or last-minute corrections.
Best-Practice Discharge Planning Starts on Day One
One of the most common audit mistakes is treating discharge planning as an afterthought. In reality, payers expect discharge planning to begin at the first treatment plan.
Best-practice IOP and PHP workflows document:
- Anticipated length of stay
- Step-down criteria
- Aftercare needs and referrals
- Patient readiness for transition
By building discharge planning into the treatment lifecycle, documentation naturally reflects clinical intent and continuity of care—rather than appearing rushed or retroactive during an audit.
Standardizing Documentation Across Clinicians and Locations
As programs grow—adding clinicians, locations, or service lines—documentation inconsistency becomes a serious risk.
Standardization doesn’t mean rigid or impersonal notes. It means ensuring every clinician captures the required elements, regardless of where or how they work.
Valant supports this by providing:
- Role-specific documentation templates
- Consistent level-of-care definitions
- Unified treatment planning structures
- Shared workflows across locations
This creates audit-ready consistency while still allowing clinicians to practice with autonomy and professionalism.
Using Level-of-Care Tracking to Prove Medical Necessity
Level-of-care decisions are central to IOP and PHP audits. Payers want to see not just what level of care was delivered, but why it was appropriate—and when transitions occurred.
Level-of-care tracking software helps providers:
- Document admission criteria clearly
- Record changes in clinical status
- Justify continued stay or step-down
- Align documentation with utilization review
When these decisions are tracked inside the EHR, audits become far less intimidating. The story of care is already there—clearly documented and easy to support.
What Discharge Planning Software Must Support
Effective discharge planning software should support more than a final note. It should help teams:
- Coordinate step-down services
- Document referrals and follow-up care
- Summarize treatment progress and outcomes
- Capture patient readiness and engagement
This ensures continuity of care while also satisfying payer and audit expectations.
What Should Be Included in IOP Discharge Summaries
When discharge summaries are structured and standardized, audits become straightforward—and providers can demonstrate both clinical quality and compliance with confidence.
A strong IOP discharge summary typically includes:
✔️ Dates of service and level of care
✔️ Reason for admission and discharge
✔️ Summary of treatment provided
✔️ Patient progress toward goals
✔️ Medications and coordination of care
✔️ Aftercare plan and referrals
Confidence Built Into Daily Workflows
Audits don’t have to be stressful. When documentation, utilization review, and level-of-care tracking are built into everyday workflows, compliance becomes a byproduct of good care—not an extra burden.
That’s exactly what Valant’s IOP/PHP Software was designed to support. With integrated scheduling, billing, utilization review, level-of-care tracking, and institutional workflows, providers can confidently meet payer and state requirements while focusing on what matters most: patient care.
Because when your documentation stands up, your program—and your patients—can keep moving forward with confidence.
Want to learn more? Check out our guide on internal vs. external audits for mental health practices.
The Best Practice Guide for IOP/PHP
Gain access to The Best Practice Guide for Intensive Outpatient Programs and Partial Hospitalization Programs: