Intake and Assessment Automation Features
Built-in Clinical History Forms
Simplified patient data collection with seamlessly integrated clinical history forms.
One-time and Scheduled Assessment Collection
Patient-reported measures save clinical session time and drive short and long term insights.
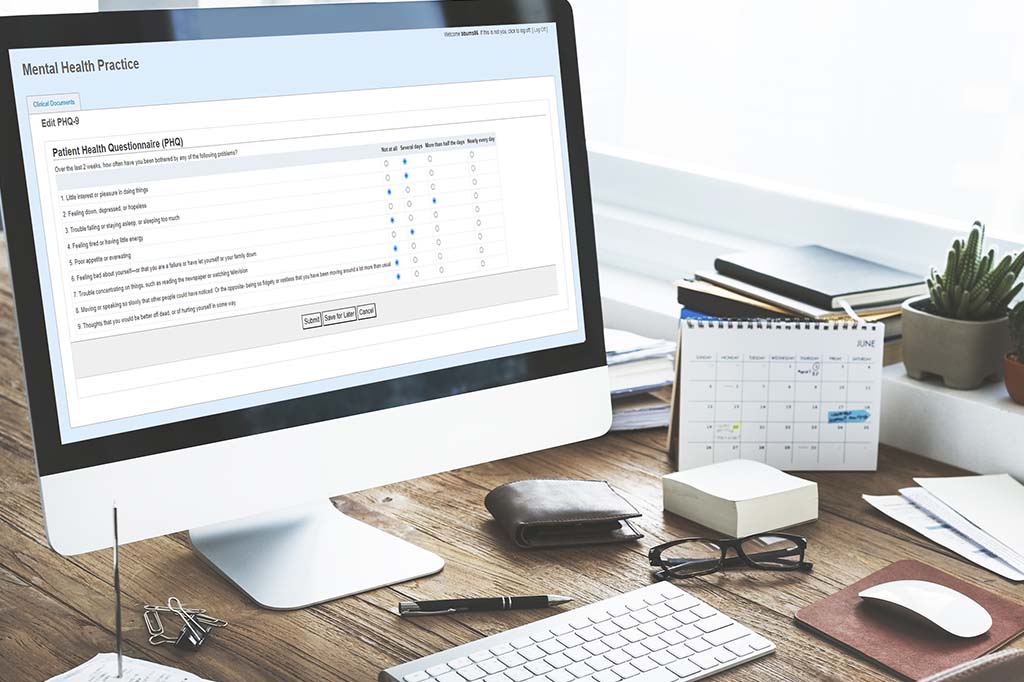
80+ Auto-scored Outcome Measures
Behavioral health assessments auto-score and graph over time for efficient treatment planning.
Flexible Packets for Intake
eSignature and read-only forms can be assembled in multiple packets, adaptable to practice needs.
eSignature Tracking
Worklists identify patients with open and overdue eSignature requests to identify who needs follow up.
Seamless eSignature Integration
Effortless digital signatures for paperless consent through one simple, secure system.
Learn a Client’s History Before You Meet Them
One of the best ways to maximize efficiency at your practice is to collect information on new clients ahead of the first appointment. Digital patient-led onboarding makes this possible.
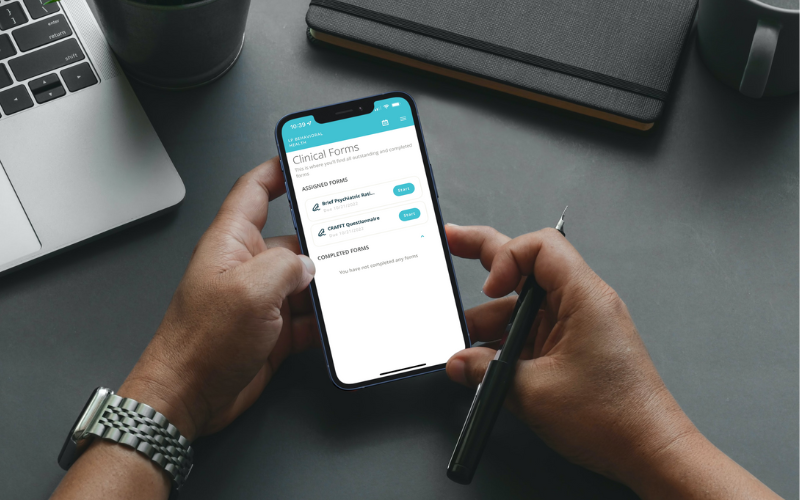
With Valant’s automated intake and assessment features, clients can complete their own onboarding process through a MYIO patient portal account. They provide their clinical history, e-sign consent forms, and fill out assessments online before their first clinical visit. This saves you time on the intake process so the patient’s first visit can be spent on treatment planning, not data gathering.
Need customized intake forms? No problem. Easily build and upload your own forms and paperwork, including signature fields.

Schedule Ongoing Assessments Ahead of Time
Outcome measures can be set to auto-send to patients’ MYIO accounts before their appointments, so you don’t have to keep track of sending outcome measures to scheduled patients or spend time during sessions completing assessments. Valant’s short clinical forms utilize box-checking to make ongoing assessments of their mental health journey fast and painless for clients.
See How One Large Practice Used Valant’s Automated Outcome Measures to Grow Revenue by 140%
“Having a superior EHR that seamlessly integrates clinical notes, scheduler, and billing, had allowed us to rapidly expand our already large organization, more than doubling our size in just a few years from 3 outpatient offices to 10 across two states.”
Developed for Behavioral Health
Valant’s intake and assessment feature was designed by clinical experts in the field of behavioral health to capture all the information you need—and none that you don’t. You won’t have to wade through the “extras” that generalist EHRs include for physical health providers. Our pre-created clinical history form knows which questions to ask in a behavioral health context.
Valant also understands the intricacies of caring for your littlest patients, so we offer a child-specific clinical history form and symptom screener.


Walk Into A First Appointment Prepared
Valant populates the information from an intake form directly into your clinical notes, so you don’t have to burn chunks of your first appointment filling in the background for yourself. Walk into every first meeting with the client’s medical and family history, symptom screening, self-harm risk assessment, and more already in hand.
The intake feature populates clinical notes with the exact answers clients provided on the form, so the nuances don’t get lost. And no, patients don’t always disclose everything at a first appointment—that’s why the auto-filled notes are completely editable. Return to update them at any time as new information emerges in your treatment sessions.
Screening Tools for Preliminary Assessment
The intake process presents an opportunity to screen clients for underlying issues they may not even be aware of Valant’s intake forms also assess symptoms of common behavioral health diagnoses, and flags items that you may want to investigate.
You can begin to form treatment ideas before the appointment, rather than react to new information off the cuff in front of your brand-new client. This proactive approach increases your confidence, which helps you built rapport at first meetings and increases your retention rate.
Prescreening also helps you assess whether an individual is a good fit for you or should see a different provider.
Ready to Get Started?
See Other Ways Valant Can Improve Clinical Care
What They’re Saying
Related Resources


Proposed Social Media Warning Labels: What Behavioral Health Providers Should Know


