Claim Assist Features
Claim Assist enables your practice to reduce review time by up to 90%,
accelerate submissions, and free your practice to grow without increasing overhead.
Automated Charge Review
Eliminate manual charge checks by automating the review process against 100+ behavioral health-specific billing rules.
Program-Specific Billing Rules
Select or create payer- and program-specific rules that automatically catch and correct coding errors before submission.
Institutional Claim Bundling
Bundle services and submit 837i institutional claims to streamline IOP/PHP billing.
Error Detection & Correction
Identify missing or incorrect data before claim submission to reduce rejections and maximize reimbursements.
Batch Claim Edits
Resolve errors that need to be reviewed prior to claim submission with an organized worklist.
Customizable Billing Rules
Leverage our extensive library of billing rules and tailor them to fit your practice’s unique payer requirements.
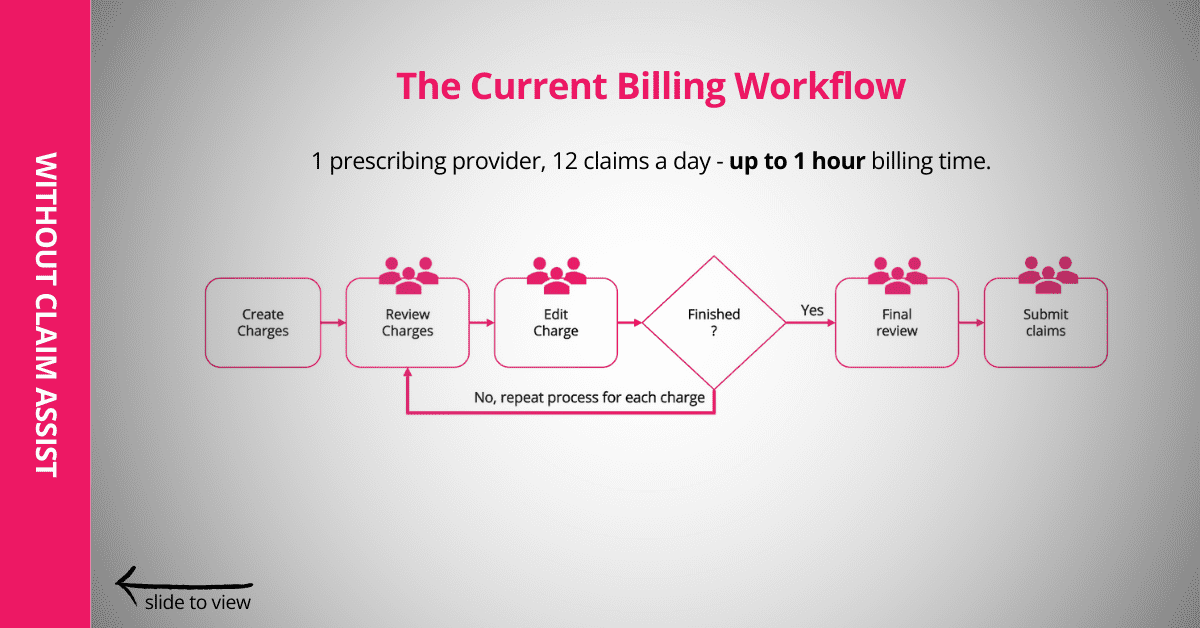
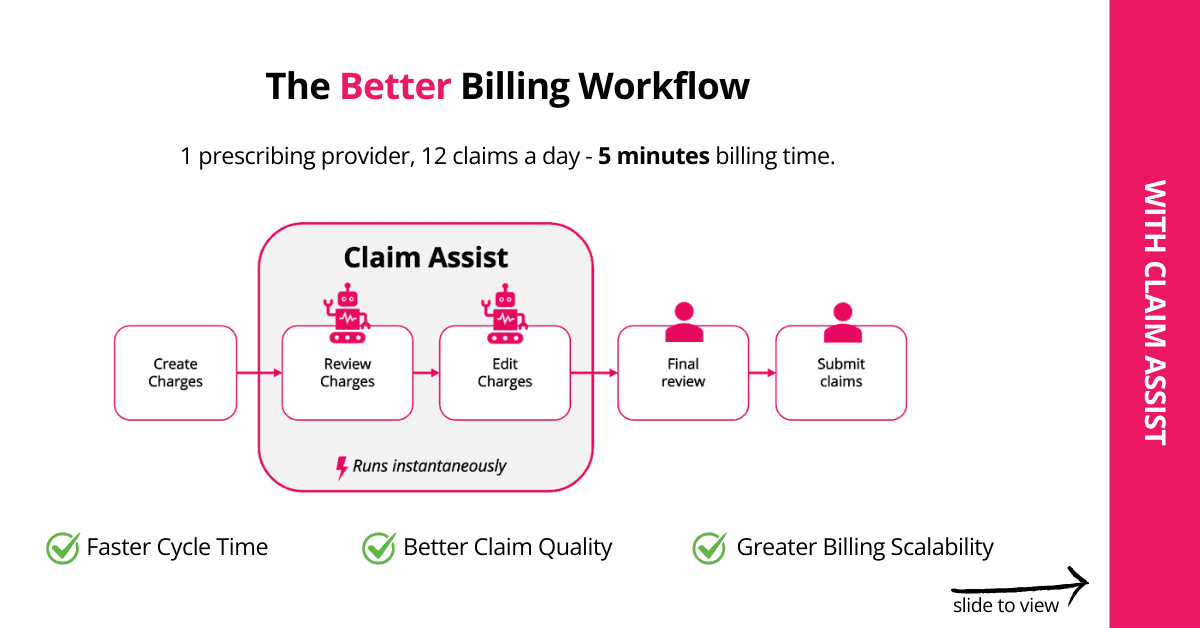
How Claim Assist Works
Claim Assist checks charges for errors, auto-fixes charges with preset rules,
and flags only claims needing special attention for billers to review.
See a before and after workflow example of a practice with Claim Assist.
What You Can Do With Claim Assist
Speed up submissions, reduce errors, and improve staff cognitive load with a billing agent that automatically reviews and edits charges based on behavioral health billing rules.
What Types of Practices Benefit From Claim Assist?
Growing practices looking to scale billing without adding staff.
Practices accepting multiple payers with different rules for services such as incident-to billing.
Billing teams managing the revenue cycle for multiple service lines or programs.
Expand Your Practice With Less Overhead
Claim Assist streamlines behavioral health billing by automating claim reviews and applying payer-specific rules, reducing review time by up to 90% and accelerating submissions — enabling your practice to grow without increasing overhead.


Designed Purpose-Built for IOP/PHP Billing
IOP and PHP add complexity to the billing process. Claim Assist simplifies it by letting you build customizable billing rules that flag and fix coding errors automatically. The system also supports bundled billing, enabling you to generate and submit institutional claims directly. Together, these tools reduce denials, speed reimbursement, and keep IOP/PHP billing as smooth as outpatient workflows.
Cut Denials and Rejections With Automated Accuracy
If your practice doesn’t have the capacity to manually review every charge, you may face frequent denials and rejections. Claim Assist changes that by automatically identifying and correcting errors before claims are submitted.

How to Successfully Negotiate with Payers for Increased Reimbursement Rates
Achieve pay for performance in behavioral health and learn how to better position your practice to renegotiate with payers for increased reimbursement.
See Other Ways Valant Can Improve Your Administrative Efficiency
What They’re Saying
Related Resources





