Explore AI Notes Assist Features
AI Notes Assist reduces documentation time and supports accurate CPT coding, giving clinicians more time to focus on care and growth.
Ready To Reclaim Your Time?
AI Notes Assist reduces documentation time and supports accurate CPT coding, giving clinicians more time to focus on care and growth.
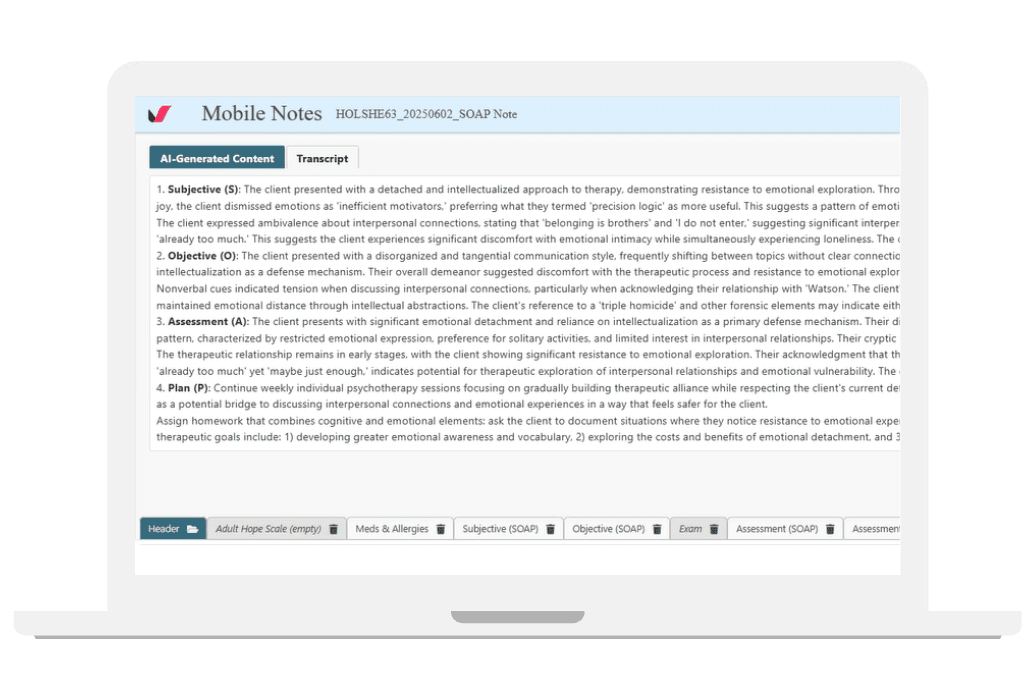
Generate clean, structured notes from your session transcripts, with CPT code suggestions that match what you document. Review and sign in minutes.
Transcribe telehealth visits automatically and receive CPT code and modifier suggestions that help prevent missed requirements.
Record in-person sessions securely and get transcripts with CPT-aligned note suggestions, all within your EHR.
AI Notes Assist was shaped by clinicians who understand the pace of behavioral health and the pressure of documentation. Their real-world experience ensures the tool supports accurate notes and trustworthy CPT code suggestions.
Created and vetted by providers who know your patients and your workflow, AI Notes Assist helps you document with confidence.


No extra copy-paste. No extra apps. Just accurate notes and CPT code support inside your secure EHR.
Skip the switching between tools. AI Notes Assist is fully integrated with Valant EHR, so telehealth, treatment planning, scheduling, billing, AI Notes Assist and more all stay in one place:
Stay productive and confident in your documentation without ever leaving Valant.

You stay in control. AI Notes Assist supports your voice and your clinical judgment by helping you start notes faster and surfacing CPT code suggestions based on what you document. After a long session, a blank page shouldn’t slow you down.
With AI Notes Assist, you’re never starting from scratch.
Put growth into practice by reducing burnout and reclaiming your time.
Gain insight from 167 behavioral health professionals on AI adoption, concerns and perceived benefits.


Valant EHR is built for practices who are interested in:
Growing
Building a thriving practice
Starting
Launching a new practice
Optimizing
Creating efficiency in your practice
Valant EHR is built for the unique workflows, billing requirements, & documentation needs of behavioral health clinicians and their practices.