For Intensive Outpatient (IOP) and Partial Hospitalization Programs (PHP), attendance is more than an operational metric—it’s a clinical signal. Missed sessions can indicate disengagement, emerging risk, or breakdowns in transitions between levels of care. And when attendance tracking lives in spreadsheets, whiteboards, or disconnected calendars, those signals are easy to miss.
IOP and PHP programs are designed to provide structure, consistency, and support during some of the most vulnerable phases of a patient’s recovery. But without reliable group scheduling and attendance tracking, even the strongest clinical models can falter. Patients fall through the cracks, transitions break down, and continuity of care suffers.
The good news?
These challenges aren’t inevitable. With the right IOP/PHP-ready EHR and group management tools, providers can proactively identify no-show risk, manage complex group rosters, and maintain continuity of care across all settings.
This is how smarter scheduling and attendance tracking help no-show proof your IOP and protect patient outcomes.
Why Attendance Tracking Is a Clinical Imperative in IOP and PHP
In group-based programs, attendance tells a story long before a crisis occurs. A missed session here, a late arrival there… patterns emerge quickly. When programs have timely visibility into those patterns, clinicians can intervene early and adjust treatment plans before disengagement becomes dropout.
An effective way to track IOP attendance and no-shows starts with automation. Attendance should be recorded from group schedules as part of daily workflows—not manually entered after the fact.
When attendance is tied to specific groups, clinicians, and levels of care, programs gain immediate visibility into:
- Patients who are missing sessions or disengaging
- Groups with declining participation
- Utilization trends across programs and locations
Instead of reacting after a patient disappears, teams can respond while there’s still time to help.
What an EHR Must Include to Support Continuity Across Levels of Care
IOP and PHP don’t exist in isolation. Patients often move between outpatient, IOP, PHP, and inpatient care—sometimes multiple times. Each transition is a potential risk point.
An EHR for intensive outpatient and partial hospitalization programs must support level-of-care transitions and continuity of care by keeping everything in one environment. That means:
- Shared patient records across all levels of care
- Attendance and participation history that follows the patient
- Documentation that remains connected through transitions
- Clear visibility into where the patient has been and where they’re going next
When data fragments across systems, continuity breaks. When it’s unified, care teams stay aligned.
Structuring PHP → IOP → Outpatient Transitions Without Losing Follow-Up
One of the most common drop-off points happens during step-down transitions. A patient completes PHP, starts IOP, and then… follow-up slips.
A structured transition process begins on day one. The most effective programs:
- Document anticipated step-down pathways in the initial treatment plan
- Track participation trends to inform readiness for transition
- Schedule future IOP or outpatient appointments before discharge
- Maintain visibility into attendance after transition
When scheduling, documentation, and discharge planning live in the same system, transitions become intentional—not reactive.
Managing Dynamic IOP Group Rosters Without Chaos
IOP groups are rarely static. Patients join mid-cycle, pause treatment, step down early, or shift tracks based on clinical need. Managing these changes manually is a recipe for errors.
Software tools that support IOP group roster management should allow staff to:
- Add or remove patients from groups without breaking the series
- Track attendance accurately across changing rosters
- Maintain historical participation records
- Adjust schedules without double-booking clinicians
This flexibility ensures that group management reflects real-world care—not rigid scheduling rules.
Supporting Multiple Levels of Care in One Behavioral Health EHR
Many programs still rely on different systems for inpatient, PHP, IOP, and outpatient care. The result? Disconnected data, duplicated work, and missed handoffs.
A multi–level-of-care behavioral health EHR supports inpatient, PHP, IOP, and outpatient in one environment—giving teams a complete view of the patient journey. Attendance, documentation, scheduling, and discharge planning remain connected, regardless of where care is delivered.
This continuity is especially critical for patients moving between structured programs and less intensive outpatient care.
Discharge and Aftercare Planning That Actually Sticks
Discharge is not an endpoint—it’s a handoff. And too often, aftercare plans live in PDFs or notes that never translate into action.
Effective discharge planning software for behavioral health should:
- Track aftercare appointments and referrals
- Connect patients to outpatient providers before discharge
- Maintain visibility into follow-up attendance
- Keep care teams informed if patients disengage
When aftercare planning is integrated into the EHR, continuity of care extends beyond the walls of the program.
Tracking Continuity of Care and Patient Outcomes Through Attendance Insight
Patients enrolled in IOP and PHP are in a vulnerable phase and require more structure than traditional outpatient therapy. During this critical phase, gaps in visibility can quickly lead to missed sessions, disengagement, and breakdowns in continuity of care as patients move between levels of care.
With clear attendance insight and connected documentation, care teams can more easily identify who is staying engaged, who may be struggling, and when additional support is needed. When participation data and progress notes remain connected throughout the patient journey, continuity of care is preserved as patients transition between IOP, PHP, and outpatient care.
The result is stronger engagement, fewer drop-offs, and better outcomes for patients who might otherwise disengage from care.
Using Attendance Data to Adjust Treatment in Real Time
“Attendance is often the first sign that a patient is struggling. When you can see it early, you can act early.”
Attendance data isn’t just administrative—it’s clinical insight. By monitoring participation in IOP group therapy over time, clinicians can:
- Identify disengagement early
- Adjust treatment intensity
- Modify group assignments
- Initiate outreach before dropout
When attendance trends are visible and actionable, treatment plans stay responsive to patient needs.
Making Transitions Between IOP and Outpatient Seamless
Reliable tracking of transitions between IOP and standard outpatient care ensures nothing falls through the cracks. The best systems allow teams to see:
- When a patient steps down
- Whether follow-up appointments were scheduled
- If attendance continues post-transition
This visibility closes the loop between programs and strengthens long-term outcomes.
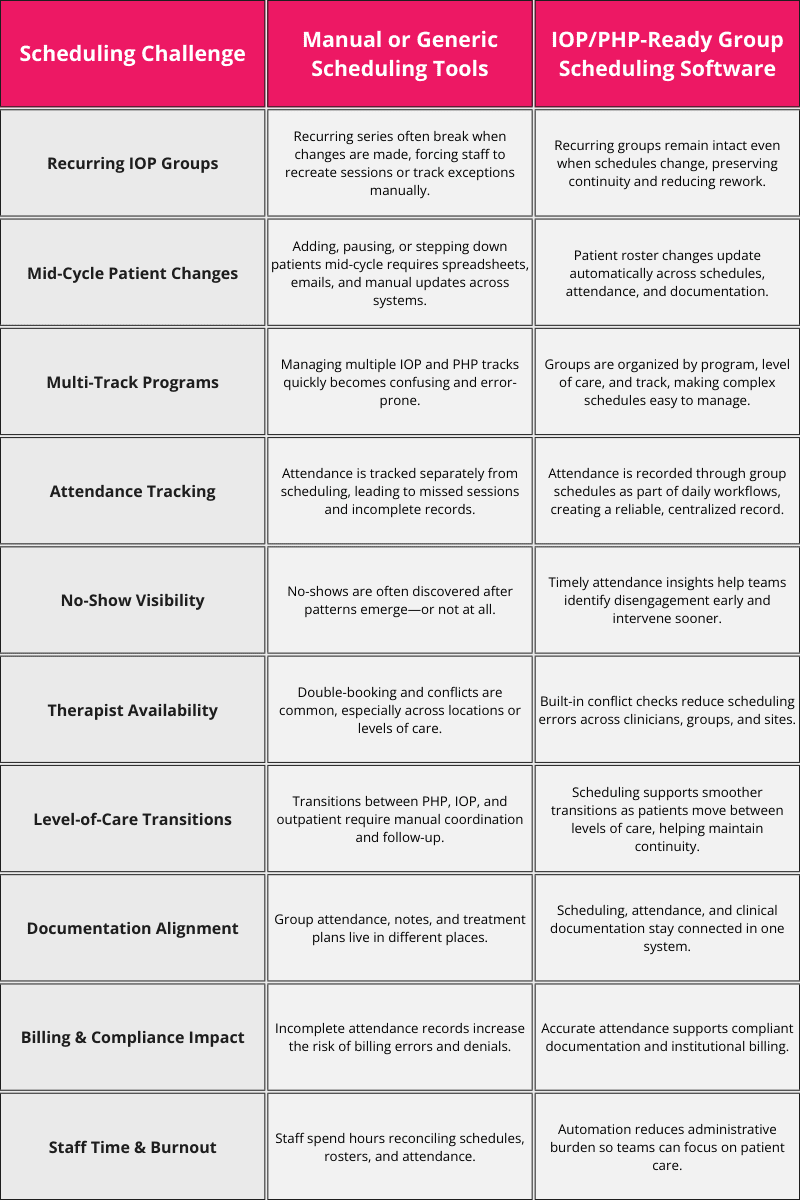
Group Scheduling Complexity: Manual Workarounds vs. IOP/PHP-Ready Software
Key Features of Group Scheduling Software for IOP and PHP
Behavioral health group scheduling software must handle complexity without creating friction. Key features include:
- Recurring group scheduling that supports changes without breaking series
- Conflict detection to prevent double-booking
- Multi-location and multi-track support
- Clear visibility into group capacity and rosters
When scheduling works the way programs actually operate, staff spend less time troubleshooting and more time supporting patients.
Bring Consistency Back to Group-Based Care
No-shows, missed transitions, and fragmented scheduling don’t have to be the cost of running IOP and PHP programs. With the right tools, attendance becomes visible, transitions stay intentional, and patients remain connected through every level of care.
Valant’s IOP/PHP Software gives your team a single system for group scheduling, attendance tracking, documentation, and level-of-care management—so continuity of care doesn’t depend on spreadsheets or manual workarounds.
The Best Practice Guide for IOP/PHP
Gain access to The Best Practice Guide for Intensive Outpatient Programs and Partial Hospitalization Programs: