Mental health progress notes, also known as clinical notes or treatment notes, are a key part of every behavioral health practice. Progress notes are where you record information about treatments applied and how the patient responds to treatment. The information recorded may include symptoms, medical history, test results, diagnoses, treatment plans, prescription medications, and progress made at appointments. This information is shared with insurance companies to justify claims. Progress notes also protect you by providing a paper trail to explain what you did for the patient as a practitioner.
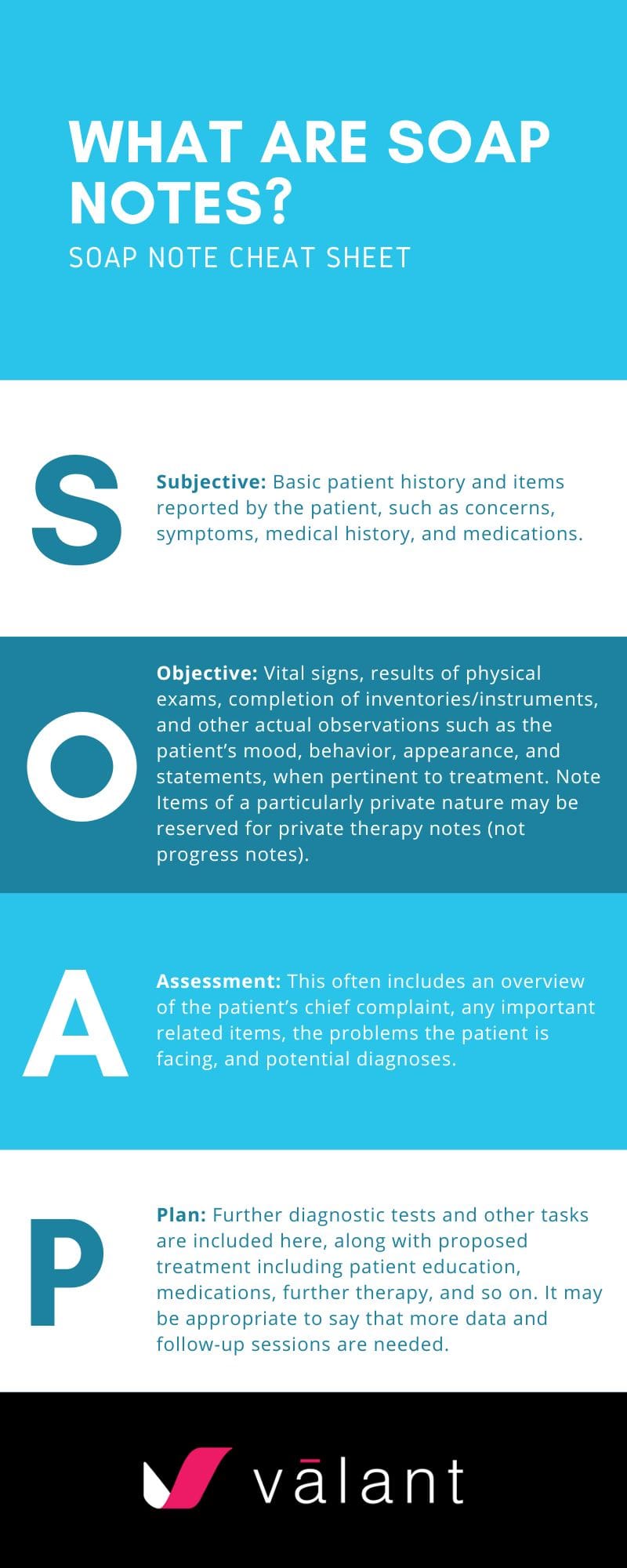
So, what is SOAP? Many behavioral health providers use SOAP every day. It’s an acronym that stands for Subjective data, Objective data, Assessment, and Planning. SOAP is one of the most popular ways to organize progress notes for therapy.
Note: Progress notes are distinct from therapy notes, which are private notes (not shared with payors). It is possible to use the SOAP structure in both types of notes, but SOAP is more commonly used to provide structure in progress notes. You can learn more about therapy notes here.
Benefits of Using SOAP Notes for Mental Health Therapy
The SOAP structure can help you take efficient notes in your mental health therapy sessions. The structure is flexible and can be adjusted with relevant subheadings under each of the four major categories, as well as basic patient demographics, session information, and concluding notes. SOAP notes can help you stay on-track during appointments with patients and quickly complete your notetaking after the session has ended. Although it is possible to create SOAP notes on paper or in a word processor like Microsoft Word, using software specifically designed for behavioral health practices offers several advantages.
What are SOAP Notes?
The SOAP note is typically specific to one therapy session and includes information such as:
- S – Subjective: Basic patient history and items reported by the patient, such as concerns, symptoms, medical history, and medications.
- O – Objective: Vital signs, results of physical exams, completion of inventories/instruments, and other actual observations such as the patient’s mood, behavior, appearance, and statements, when pertinent to treatment. Note Items of a particularly private nature may be reserved for private therapy notes (not progress notes).
- A – Assessment: This often includes an overview of the patient’s chief complaint, any important related items, the problems the patient is facing, and potential diagnoses.
- P – Plan: Further diagnostic tests and other tasks are included here, along with proposed treatment including patient education, medications, further therapy, and so on. It may be appropriate to say that more data and follow-up sessions are needed.
Some of the above information will carry over from session to session, and the notes will typically have more data and more confidence about diagnoses and treatment plans when you are further along with a patient. Earlier sessions may be more focused on collecting more data.
How to Write SOAP Notes
SOAP notes can be written on paper or a word processor using a template, or they can be entered into an electronic health record (EHR) system. As you will often be referring to past information and carrying forward the same information to future SOAP notes for upcoming patient appointments before editing and updating the information, it can quickly become unwieldy to deal with paper or word-processor based SOAP notes.
Example
SOAP notes are quite flexible. Here is one basic example of how you might structure a SOAP note. You can also add additional sub-sections and structure as needed.
Your Practice Name
Your Practice Address (555) 555-5555
Patient:
Patient Birth Date:
Provider:
Date:
Mental Disorders:
Other Conditions:
General Medical:
Current medications:
| Medication | Dosage | Sig | Prescriber |
| Subjective Data | Disclosed by Patient:
|
Provider’s Interpretation:
|
| Objective / Observations | Pre-Existing Data (Test Results, etc.):
|
Observed in Session:
|
| Assessment | Provider’s Analysis:
|
Inferences/Concerns:
|
| Plan | Treatment Plan:
|
Specific Actions:
|
| Review | Concluding Thoughts:
|
Items for Follow Up:
|
At this point, you may want to learn about an advanced documentation solution that saves time throughout the patient care cycle. Check out Valant’s clinical documentation features to learn more. Our software can help you maximize time with your patients, while always keeping needed information secure and accessible. With Valant, you can finish your notes before the end of the session. Contact us today for a free demonstration, or to learn more about how our software can benefit your practice.
FAQ – Frequently Asked Questions
What are mental health progress notes?
Mental health progress notes, also known as clinical or treatment notes, are records that document treatments applied and the patient’s response to treatment. These notes typically include symptoms, medical history, test results, diagnoses, treatment plans, prescription medications, and progress made during appointments.
How do progress notes differ from therapy notes?
Progress notes are shared with insurance companies to justify claims and provide a legal record of the care given to patients. Therapy notes, on the other hand, are private and not shared with payors, focusing on more personal reflections and details about the therapy sessions.
What is the SOAP format in mental health progress notes?
SOAP stands for Subjective, Objective, Assessment, and Planning. It is a structured method for organizing progress notes commonly used in therapy to help clinicians track patient progress and treatment efficiently.
What information is included in each part of a SOAP note?
- S (Subjective): Patient-reported information, such as symptoms, concerns, medical history, and medications.
- O (Objective): Observable data, such as vital signs, physical exam results, mood, behavior, and appearance.
- A (Assessment): An overview of the patient’s issues, problems, and potential diagnoses.
- P (Plan): A summary of treatment plans, diagnostic tests, medications, further therapy, and patient education.
How do SOAP notes help mental health practitioners?
SOAP notes provide a clear, structured way to document each therapy session, making it easier to track patient progress, review past information, and create treatment plans. The structure allows for quicker and more organized note-taking, improving the efficiency of mental health practitioners.
Can SOAP notes be used for both progress notes and therapy notes?
Yes, SOAP notes can be used for both progress notes and therapy notes, although they are more commonly used for progress notes. In therapy notes, the SOAP structure can still be applied but with a focus on more private reflections.
What are the benefits of using software for SOAP notes compared to paper or word processors?
Using behavioral health-specific software for SOAP notes offers the ability to easily reference past notes, carry forward information from previous sessions, and streamline the notetaking process. It also eliminates the unwieldiness of paper-based systems, providing better organization and efficiency.
How do SOAP notes evolve over time with a patient?
Earlier SOAP notes often focus on gathering data about the patient, while later notes become more detailed with more confidence in diagnoses and treatment plans as the practitioner gathers more information and monitors patient progress.