Outcome measures have been talked about in the behavioral health field for over 20 years yet only 18% of psychiatrists and 11% of psychologists in the US routinely use outcome measures (Fortney, Sladek, & Unützer, 2015). There is a lot of evidence that suggests that using outcome measures to track and provide feedback on patient progress is linked to better outcomes.
Outcome measures are tools, often rating scales, delivered systematically to measure the impact of a service or intervention on a patient’s mental health status. Outcome measures, in conjunction with clinical treatment, give providers a full view of the patient’s response to treatment, deeper insight into patient deterioration, analysis into how the practice is performing, and demonstrated value to insurance carriers.
Outcome measures have been talked about in the behavioral health field for over 20 years yet only 18% of psychiatrists and 11% of psychologists in the US routinely use outcome measures (Fortney, Sladek, & Unützer, 2015).
Best Practices for Using Rating Scales to Measure Mental Health
Rating scales, sometimes called progress monitoring tools, stand among the easiest outcome measures to implement within a practice. A good rating scale will have a strong scientific foundation, and along with being practical, reliable, and valid, will be sensitive to patient changes. It’s a good thing many of these have been around for years and have been psychometrically validated. Most rating scales today are easy to administer and interpret on an ongoing basis.
When using rating scales there are a couple of best practice guidelines:
- Feasibility: Invest in an EHR system to make rating scales simple to administer. They can be sent digitally for the patient to complete at their convenience, securely, and delivered digitally back to the office where answers automatically flow into the patient’s chart and notes—in a graphical format too—for review.
- Frequency: A rating scale for outcome measures isn’t going to work if only given once or sporadically. In order to track how a patient is responding to treatment, a rating scale may be given before every appointment or some other regular interval. This allows for the development of trends, greater self-awareness, and analysis that may lead to additional diagnoses.
- Adjusting the health treatment plan: One of the most important pieces of the puzzle is to actually use this actionable patient intelligence. Review the graph and charts with the patient to show progress. Patients perceive symptom rating scales to be efficient, complementary of their provider’s clinical judgment and as evidence that their providers are taking their behavioral health problems seriously (Fortney, Sladek, & Unützer, 2015 page 21).
Benefits of Using Outcome Measures in Behavioral Health
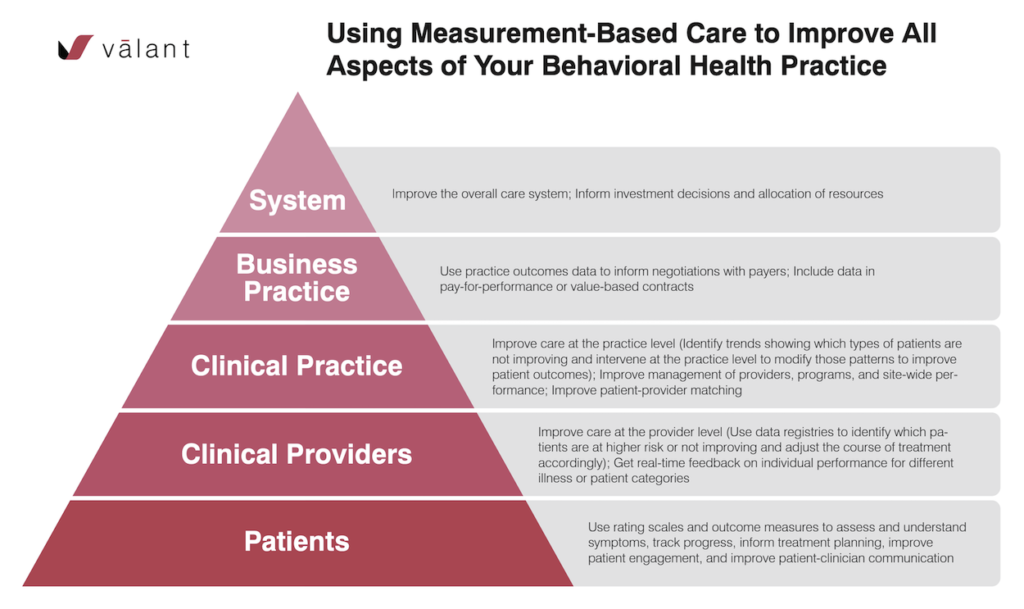
With the right technology, the cost and effort of managing patient-reported symptom rating scales are minimal, yet the benefits of outcomes-based care apply to patients, providers, and payers alike in a very big way.
For patients:
- Improve outcomes: A study published in the American Journal of Psychiatry showed that simply measuring response to treatment increased depression remission rates from 29% to 74%.
- Validates feelings: Reviewing rating scales with a provider can help validate how the patient is feeling as it provides tangible evidence for something that the patient experiences subjectively.
- Empowers communication: Helps patients feel more involved in decision-making.
- Greater understanding: Patients have more knowledge about their disorder and symptoms.
- Recognizes early treatment improvements: Visualizing data can be a powerful tool in patient motivation and engagement. If they see they are getting better over time, they are reinforced for adhering to their treatment plan.
Patients perceive symptom rating scales to be efficient, complementary of their provider’s clinical judgment and as evidence that their providers are taking their behavioral health problems seriously (Fortney, Sladek, & Unützer, 2015 page 21).
For providers and their organization:
- Focused patient treatment: Allows the provider to determine and concentrate on the most severe symptoms first. Providers are empowered to more closely evaluate and fine-tune treatment plans.
- Greater clinical effectiveness: Provides an opportunity to assess progress and adjust treatment more quickly and in a more targeted fashion.
- Better patient partnership: Improves patient cognizance of the warning signs of relapse or recurrence and correlates of success
- Recognition: Allows practices to demonstrate the success and value of their work.
- Enables value-based care: Increasingly, measurement-based care and outcomes data are being incorporated into value-based care contracts.
- Increased collaboration: Enables informed coordination across providers within an organization, as well as more efficient communication about progress with collaborating providers outside of the organization.
For payers:
- Promotes transparency and accountability: Rating scales can make patient outcomes more transparent and help payers recognize quality.
- Separates the cream of the crop: Helps identify providers who are generating the best outcomes.
- Helps payers better allocate resources to drive better clinical outcomes: In partnership with providers, payers will have better insight into what types of services work best for various populations and which providers produce the best outcomes. This will allow payers to make better decisions about where to make investments.
- Helps lower costs on the physical health side: Many studies have shown that healthcare costs are significantly higher if a patient has a mental health disorder comorbid with a chronic medical condition. Increasingly, payers appreciate that effectively treating mental health disorders is critical to bending the cost curve. Outcome measures will help them make the connection between behavioral health and physical health outcomes and attract more investment to behavioral health service delivery.
Top Rating Scales for Behavioral Health
There are many validated rating scales that providers can easily implement. The following list incorporates some of the more common scales:
- Depression = PHQ-9
- Generalized Anxiety Disorder = GAD-7
- Panic Disorder = PDSS
- Social Anxiety Disorder = SPIN
- PTSD = PCL-C
- Alcohol Use Disorder = AUDIT
- Drug Use Disorder = NIDA-Modified ASSIST
- ADHD = ASRS
- OCD = YBOCS
- SCARED for Child Anxiety disorders
- Vanderbilt for ADHD and other disorders of childhood
The Kennedy Forum provides a more comprehensive list in its Measurement Base Care supplement.
Do not feel overwhelmed by this list. As a provider, it isn’t necessary to implement every scale at once. Start small with one or two of the more reliable and valid like PHQ-9 and GAD-7. These rating scales can be given to every patient to establish a baseline. It is more important as a provider to focus on frequency and consistency.
Getting Started Using Outcome Measures
A robust EHR with integrated outcomes-based care functionality can handle the majority of the administrative workload, allowing the practice to enjoy the benefits of outcome measures without becoming overwhelmed by extra tasks.
Valant, for example, automates the administration of outcome measures and other screening tools as integrated parts of patient engagement and clinical documentation. Over 80 rating scales come standard in Valant’s EHR for Behavioral Health. Once a patient completes a survey, it flows into the documentation area where the outcome measurement engine scores and summarizes the results into a clinical narrative. The provider can then select which clinical interventions to utilize and roll it up into a document that summarizes the treatment plan in a condensed format which can be shared with the patient.
The use of outcome measures and rating scales will improve your practice, patients, and payer relationships. The most important step to take is to simply start using some sort of outcome measurement. Start small with one or two rating scales across all your patients. You will see immediate results as patients feel more empowered and validated, treatment becomes more focused, and payers have better visibility into your patient outcomes.
See How to Automate Outcome Measures
Want to see how Valant’s Behavioral Health EHR automates the administration of outcome measures?