Data equals knowledge. Good clinical data provides the irrefutable evidence that goes beyond our assumptions and observations to give us actionable intelligence. Data keeps us from wasting time and resources.
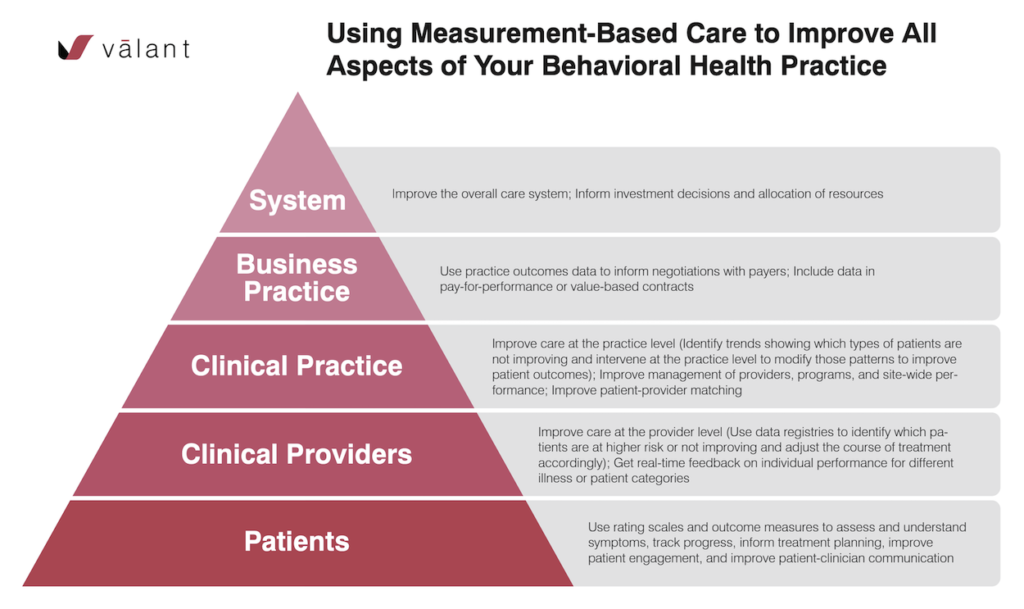
Clinical data in the behavioral health industry allows clinicians to establish patient baselines and benchmarks that can be used in setting up goals and treatment plans that lead to better patient outcomes. This clinical data can be used at every level—patient, provider, practice, payer, and system—to not only inform decisions but to negotiate better pay, to measure performance, and measure effectiveness.
Where Does the Clinical Data Come From?
It’s important to know where to get the data. It isn’t like the physical health industry where patient baselines are established as soon as they walk through the door. Every doctor visit comes with the standard height, weight, and blood pressure diagnostic. Blood tests measure many physical health diagnoses like diabetes, hypertension, and cholesterol. Scans help measure the presence and size of physical abnormalities inside the body.
These kinds of measurements are completely lacking in behavioral healthcare.
Or are they?
Outcome measures are the best indicators of how a patient is doing when they visit a behavioral health clinician. These rating scales, delivered systematically, measure the impact of a service or intervention on a patient’s mental health status. There are many validated symptom rating scales available to use like the PHQ-9 for depression or the GAD-7 for anxiety. Rating scales are easy to administer, trend over time, and provide the clinical data for a patient’s baseline improvement or decline.
Using Clinical Data to Improve All Aspects of the Behavioral Health Practice
Over the last several years, measurement-based care has become a crucial means for the aggregation and downstream use of outcome measurement data in behavioral health. Measurement-based care allows clinicians to use outcome measures during all phases of care to help with assessment, track clinical progress, and inform treatment decisions.
At the outset, the core benefit of measurement-based care is really to the patient and clinician. However, as more clinical data is collected, it can be used in higher levels within the system to improve treatment outcomes and create a marketplace for quality at scale.
Using Clinical Data to Improve Patient Engagement
In research from Fortney, et.al. 2016, they analyzed studies with nearly “300 therapists and more than 6,000 patients and found that those randomly assigned to measurement-based care had significantly and substantially better outcomes than patients randomly assigned to usual care.”
As a clinician, simply sharing the results of outcome measures empowers communication, validates feelings, and provides patients with greater knowledge about their disorders. It also helps recognize early treatment improvements or deteriorations so the treatment plan can be adjusted accordingly.
Using Data to Improve Clinical Care
With the consistent use of clinical data, better care can be provided at both the provider and practice levels. Data can be gleaned from the clinical registries pulled from the EHR system. This data allows a clinician to focus patient treatment, often providing insight into the most severe symptoms. This data also delivers greater clinical effectiveness by providing opportunities to assess patient progress more often and adjust treatment strategies more quickly and in a more targeted way.
When there are multiple providers in a practice, the clinical data can be reviewed at the practice level to identify trends and correlate the types of patients and/or interventions that are– or conversely, are not– improving patient outcomes. Over time, the data can help identify if there are improvement opportunities within a specific program or training opportunities for individual providers. And it can inform your patient-provider matching to optimize outcomes at a practice level.
Using Clinical Data to Run a More Profitable Behavioral Health Practice
Clinical data provides owners and practice managers with the tools they need to improve business outcomes and run a more profitable practice. Quality metrics provided by rating scales promote transparency and accountability to payers who can better allocate resources to drive better clinical outcomes. Payers gain better insight into which type of services work best for different populations and where to spend their investment dollars.
There are several studies available that show significantly higher healthcare costs if a patient has a mental health disorder comorbid with a chronic medical condition. Payers appreciate the lower healthcare costs that come with effectively treating behavioral health disorders.
Finally, the data collected allows clinicians to better negotiate reimbursement rates. When payers see that practices are tracking quality metrics like patient outcomes and time-to-appointment, they are willing to reimburse more.
Using Clinical Data to Systematically Improve Behavioral Health
The industry is ripe for an overhaul. As the system begins to widely adopt the measurement-based care model, the goal for every practice should be regular measurement for every client. This is called universal measurement. Universal measurement creates an opportunity for quality improvement across behavioral healthcare at scale because of the proven relationship between measurement-based healthcare and better behavioral health outcomes.
The patient data collected through outcome measures can be used to improve decision making at every level including what is referred to as clinical-decision support. Universal measurement also creates an opportunity to lower healthcare costs across the board because of the well-documented relationship between behavioral health and physical health outcomes.
Universal measurement helps differentiate and create a marketplace for quality while creating greater investment in behavioral healthcare services. It isn’t just about moving dollars around between pie pieces anymore. The pie will grow. It will enable us to systematically address the current state of underinvestment in the industry.
Tiny Steps Lead to Great Rewards
They say the first step in any journey is always the hardest. The hardest part about gathering the clinical data is to make the commitment to do it and making the infrastructure investment to support it.
Adopting a measurement-based care philosophy can be boiled down to the following steps:
- Invest in a purpose-built EHR that can automate the data-collection process
- Use the right rating scales in the practice to gather the data
- Educate everyone involved in a patient’s treatment about measurement-based care and why you are doing it
- Set goals
Once the pieces are in place, a door is opened to a whole new world of improved patient engagement, elevated clinical care, increased practice profits, and increased industry standards.
The Right Tools Make the Job Easy
For behavioral health practices committed to providing measurement-based care, Valant is the right tool for the job. It automates the administration of outcome measures and other screening tools as integrated parts of patient engagement and clinical documentation. Once the clinical data is collected, you can begin to analyze it. Valant allows you to generate, download and print a variety of reports, giving you actionable insights by patient types, providers, facilities, diagnoses, symptom severity, etc.
Learn how to put your data to work for you.